Non Insertional Achilles Tendonitis
Overview
 Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Causes
Unusual use or overuse of the lower leg muscles and Achilles tendon is usually the cause of Achilles tendinitis. Repetitive jumping, kicking, and sprinting can lead to Achilles tendinitis in both recreational and competitive athletes. Runners, dancers, and athletes over age 65 are especially at risk. Sudden increases in training or competition can also inflame your Achilles tendon. For example, adding hills, stair-climbing, or sprinting to your running workout puts extra stress on your Achilles tendon. Improper technique during training can also strain the tendon. Intense running or jumping without stretching and strengthening your lower leg muscles can put you at risk regardless of your age or fitness level. Running on tight, exhausted, or fatigued calf muscles can put added stress on your Achilles tendon, as your tendon may not be ready to quickly start a workout after a period of inactivity. Direct blows or other injuries to the ankle, foot, or lower leg may pull your Achilles tendon too far and stretch the tissue. A hard contraction of the calf muscles, such as can happen when you push for the final sprint in a race, can strain the tendon. People whose feet roll inward, a condition called overpronation, are particularly at risk. Sometimes, shoes with too much heel cushioning put extra strain on the Achilles tendon.
Symptoms
Signs and symptoms of Achilles Tendinitis generally include pain and stiffness along your achilles tendon, especially in the morning. Pain in the back of your heel that gets worse with activity. Severe pain the day after exercising. Swelling that gets worse with activity. If you feel a pop in the back of your heel or bottom of you calf, you may have ruptured or torn you achilles tendon.
Diagnosis
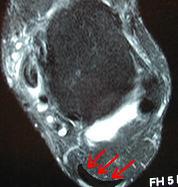
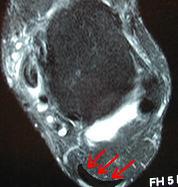
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
Achilles tendonitis will often respond to rest or changes in activity, stretching, or ice after activity. Non-steroidal anti- inflammatory drugs (NSAIDs), such as ibuprofen or naproxen may also help. Physical therapy focusing on stretching and strengthening, massage, alternating hot and cold baths, and ultrasound or sound waves can also help with healing and comfort. The temporary use of a heel lift or the insertion of an arch support, called an orthotic, into the shoe or sneaker can also help. Although seldom necessary, the ankle may be kept in a short leg cast or splint. Surgery is rarely needed but can remove bone spurs or the bony prominence of the heel bone. The injection of corticosteroids such as cortisone into the area of the Achilles tendon is usually avoided because it may cause the tendon to rupture.
Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
The following measures can significantly reduce the risk of developing Achilles tendonitis. Adequately stretch and warm up prior to exercise. Warm down and stretch after exercise. Choose footwear carefully and use footwear appropriate to the sport being undertaken. Use orthotic devices in footwear to correctly support the foot. Exercise within fitness levels and follow a sensible exercise programme. Develop strong, flexible calf muscles.
 Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Causes
Unusual use or overuse of the lower leg muscles and Achilles tendon is usually the cause of Achilles tendinitis. Repetitive jumping, kicking, and sprinting can lead to Achilles tendinitis in both recreational and competitive athletes. Runners, dancers, and athletes over age 65 are especially at risk. Sudden increases in training or competition can also inflame your Achilles tendon. For example, adding hills, stair-climbing, or sprinting to your running workout puts extra stress on your Achilles tendon. Improper technique during training can also strain the tendon. Intense running or jumping without stretching and strengthening your lower leg muscles can put you at risk regardless of your age or fitness level. Running on tight, exhausted, or fatigued calf muscles can put added stress on your Achilles tendon, as your tendon may not be ready to quickly start a workout after a period of inactivity. Direct blows or other injuries to the ankle, foot, or lower leg may pull your Achilles tendon too far and stretch the tissue. A hard contraction of the calf muscles, such as can happen when you push for the final sprint in a race, can strain the tendon. People whose feet roll inward, a condition called overpronation, are particularly at risk. Sometimes, shoes with too much heel cushioning put extra strain on the Achilles tendon.
Symptoms
Signs and symptoms of Achilles Tendinitis generally include pain and stiffness along your achilles tendon, especially in the morning. Pain in the back of your heel that gets worse with activity. Severe pain the day after exercising. Swelling that gets worse with activity. If you feel a pop in the back of your heel or bottom of you calf, you may have ruptured or torn you achilles tendon.
Diagnosis
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
Achilles tendonitis will often respond to rest or changes in activity, stretching, or ice after activity. Non-steroidal anti- inflammatory drugs (NSAIDs), such as ibuprofen or naproxen may also help. Physical therapy focusing on stretching and strengthening, massage, alternating hot and cold baths, and ultrasound or sound waves can also help with healing and comfort. The temporary use of a heel lift or the insertion of an arch support, called an orthotic, into the shoe or sneaker can also help. Although seldom necessary, the ankle may be kept in a short leg cast or splint. Surgery is rarely needed but can remove bone spurs or the bony prominence of the heel bone. The injection of corticosteroids such as cortisone into the area of the Achilles tendon is usually avoided because it may cause the tendon to rupture.
Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
The following measures can significantly reduce the risk of developing Achilles tendonitis. Adequately stretch and warm up prior to exercise. Warm down and stretch after exercise. Choose footwear carefully and use footwear appropriate to the sport being undertaken. Use orthotic devices in footwear to correctly support the foot. Exercise within fitness levels and follow a sensible exercise programme. Develop strong, flexible calf muscles.