Pain In The Foot's Arch Cause And Effect
Most flat feet are not painful, particularly those flat feet seen in children. In the adult acquired flatfoot, pain occurs because soft tissues (tendons and ligaments) have been torn. The deformity progresses or worsens because once the vital ligaments and posterior tibial tendon are lost, nothing can take their place to hold up the arch of the foot. The painful, progressive adult acquired flatfoot affects women four times as frequently as men. It occurs in middle to older age people with a mean age of 60 years. Most people who develop the condition already have flat feet. A change occurs in one foot where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Why this event occurs in some people (female more than male) and only in one foot remains poorly understood. Contributing factors increasing the risk of adult acquired flatfoot are diabetes, hypertension, and obesity.

Causes
Often, tarsal tunnel syndrome is misdiagnosed and confused with plantar fasciitis. Tarsal tunnel syndrome is when the tibial nerve which runs through the ankle, is pinched as it passes through the flexor retinaculum, the supportive band that surrounds the ankle joint. The symptoms of tarsal tunnel syndrome are often limited to the ankle but the since the nerve passes through the entire foot it can cause arch pain. Arch pain associated with foot strain is mainly caused by a pronated foot (rolls inward) or a flat foot. These are usually not singular causes of arch pain, but in combination with other factors, arch pain may result.
Symptoms
Common symptoms of plantar fasciitis include pain in the morning when you first get out of bed, pain and stiffness when you start to walk after sitting for a while, increasing arch or heel pain toward the end of the day, tired feet at the end of the day. Other causes of arch and heel pain include arthritis, infection, fractures and sprains, and even certain systemic diseases. Since there are multiple possible causes, you should see your podiatrist for a thorough evaluation if you are experiencing arch or heel pain that does not respond quickly to early treatment.
Diagnosis
The doctor will take a brief history to determine how the injury occurred. If necessary, a thorough physical exam may be conducted to evaluate for any other injuries. Taking your workout shoes to the exam may also provide valuable information to the medical practitioner. Both feet will be physically and visually examined by the medical practitioner. The foot and arch will be touched and manipulated possibly with a lot of pressure and inspected to identify obvious deformities, tender spots, or any differences in the bones of the foot and arch.
Non Surgical Treatment
If it is flat feet, then you'd seek professional advice and maybe need orthotics, or arch supports to prevent the pressures and to stop the pain. One of the other reasons you can get pain in this area of the foot is plantar fasciitis. The plantar fascia is a membrane that is inside of the skin and attaches to the heel bone here. It divides into three bands that go out of the foot here: the outer band, the central band, and the medial band here. Often, from impact, you get an inflammation of that attachment to the heel bone and this can often spread up the medial band and this is another way of getting pain in that arch. Now, the way to treat that is also using arch supports but also heel cushions, better soled shoes to prevent the pressure. These things normally disappear after a year, 18 months. Plantar fasciitis is easier to treat because it's not a long term problem. If you do need arch support, something like this would be very good for both problems.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Stretching Exercises
Point your toes. To ease foot pain and aching in your feet, lift one foot and roll it downward until the toes are pointed toward the ground. Then flex your foot. Repeat using the other foot. This exercise will help stretch out all the small muscles that are on the bottom of your feet, which can help relieve aching and improve blood circulation. Raise your heels. This exercise is good for relieving toe cramps caused by standing for hours in constricting shoes, says Kurtz. Bonus: It can also strengthen calf muscles and make them look more defined. Stand up and lift your heels so that you are standing on the balls of your feet. Hold for 10 seconds. Repeat 10 times. Squeeze your toes. To strengthen the toes and help alleviate foot pain from hammertoes (when a toe resembles a claw), separate your toes using corks or foam toe separators and then squeeze your toes together for five seconds. Repeat 10 times. Roll a ball. Want to create an instant massage for the bottom of your feet? Roll a golf ball or tennis ball under the ball of your foot. Apply light pressure for about two minutes. This exercise can be helpful for arch pain, cramps, and heel pain from plantar fasciitis. Stretch standing up. A weight-bearing, runners-type stretch can be helpful for foot pain in the arch. Stand up and place your toes against a wall; lean forward a little until you feel your arch stretch. Repeat using the other foot. Stretch sitting down. Sit barefoot and cross your left leg so that your ankle rests on your right thigh. Then hold your toes and bend them back toward your shin, stretching the band of tissue connecting the bottom of the heel to the ball. A University of Rochester study found that people living with plantar fasciitis had a 75 percent chance of having no pain within three to six months of performing this stretch three times daily. Give yourself a foot massage. Nothing spells pain relief like a good foot rub. Use the following technique recommended by Rhonda Crockett, a licensed massage therapist at Ohio State University?s Center for Integrative Medicine in Columbus. Start with your toes, using your thumb to massage them in circular motions. Then move to the arch under your foot and gradually work your way down to the heel, applying pressure with your fingers and palm of your hand. Use lotion to allow your hand to move smoothly over your foot. Relax in a warm bath with Epsom salts. The combination of warm water and Epsom salts will give you a double dose of pain relief and relaxation. Magnesium sulfate, the key compound in Epsom salts, has been found to relax muscles, reduce pain, and sedate the nervous system. Plus, warm water helps improve circulation in the feet and relieve muscle pain. Crockett recommends adding two cups of Epsom salts to a warm bath and soaking for 20 minutes.
An Achilles Tendon Rupture How Do I Know I Suffered One?
Overview  Achilles tendon rupture are common. Most athletes describe a sudden acute event with an associated popping sensation and pain in the Achilles tendon. They often think that they have been kicked or struck in the calf. It is important to get prompt treatment and to be placed in an equinous cast (a cast with the foot in a pointed position). More definitive treatment options can be discussed after this has occurred. Causes Ruptured Achilles tendons may result from falling from a height or down a hole. Increasing training intensity abruptly, boosting distance, frequency or duration by more than 10% a week. Failing to stretch before and after exercise. Repetitive training, especially uphill running. Deyhydration, which causes cramping and tightness in the calves. Taking antibiotics. Improper footwear. Explosive movements in competitive sports like basketball, soccer or track & field. Symptoms If the Achilles tendon is ruptured you may experience a sudden pain in the back of your leg, as if someone had kicked you, followed by, swelling, stiffness, and difficulty to stand on tiptoe and push the leg when walking. A popping or snapping sound may be heard when the injury occurs. You may also feel a gap or depression in the tendon, just above heel bone. Ruptures usually occurs in those aged 30 - 70 years, during a sudden forceful push off from the foot. Without proper healing of the tendon, you will have a permanent limp and weakness when using the leg. Diagnosis Other less serious causes of pain in the back of the lower leg include Achilles tendonitis or bursitis. To distinguish between these possibilities, your physician will take a thorough history and examine your lower leg to look for signs of a rupture. The presence of a defect in the tendon that can be felt, evidence of weakness with plantarflexion, and a history consistent with Achilles tendon rupture are usually sufficient for diagnosis. Your physician may also perform a ?Thompson test,? which consists of squeezing the calf muscles of the affected leg. With an intact Achilles tendon, the foot will bend downward; however, with a complete rupture of the tendon, the foot will not move. In cases where the diagnosis is equivocal, your physician may order an MRI of the leg to diagnose a rupture of the Achilles tendon. Non Surgical Treatment The most widely used method of non-surgical treatment involves the use of serial casting with gradual progression from plantar flexion to neutral or using a solid removable boot with heel inserts to bring the ends of the tendon closer together. The advantage of a solid removable boot is that it allows the patient to begin early motion and is removable. Wide variability exists among surgeons in regards to the period of absolute immobilization, initiating range of motion exercises, and progression of weight bearing status.
Achilles tendon rupture are common. Most athletes describe a sudden acute event with an associated popping sensation and pain in the Achilles tendon. They often think that they have been kicked or struck in the calf. It is important to get prompt treatment and to be placed in an equinous cast (a cast with the foot in a pointed position). More definitive treatment options can be discussed after this has occurred. Causes Ruptured Achilles tendons may result from falling from a height or down a hole. Increasing training intensity abruptly, boosting distance, frequency or duration by more than 10% a week. Failing to stretch before and after exercise. Repetitive training, especially uphill running. Deyhydration, which causes cramping and tightness in the calves. Taking antibiotics. Improper footwear. Explosive movements in competitive sports like basketball, soccer or track & field. Symptoms If the Achilles tendon is ruptured you may experience a sudden pain in the back of your leg, as if someone had kicked you, followed by, swelling, stiffness, and difficulty to stand on tiptoe and push the leg when walking. A popping or snapping sound may be heard when the injury occurs. You may also feel a gap or depression in the tendon, just above heel bone. Ruptures usually occurs in those aged 30 - 70 years, during a sudden forceful push off from the foot. Without proper healing of the tendon, you will have a permanent limp and weakness when using the leg. Diagnosis Other less serious causes of pain in the back of the lower leg include Achilles tendonitis or bursitis. To distinguish between these possibilities, your physician will take a thorough history and examine your lower leg to look for signs of a rupture. The presence of a defect in the tendon that can be felt, evidence of weakness with plantarflexion, and a history consistent with Achilles tendon rupture are usually sufficient for diagnosis. Your physician may also perform a ?Thompson test,? which consists of squeezing the calf muscles of the affected leg. With an intact Achilles tendon, the foot will bend downward; however, with a complete rupture of the tendon, the foot will not move. In cases where the diagnosis is equivocal, your physician may order an MRI of the leg to diagnose a rupture of the Achilles tendon. Non Surgical Treatment The most widely used method of non-surgical treatment involves the use of serial casting with gradual progression from plantar flexion to neutral or using a solid removable boot with heel inserts to bring the ends of the tendon closer together. The advantage of a solid removable boot is that it allows the patient to begin early motion and is removable. Wide variability exists among surgeons in regards to the period of absolute immobilization, initiating range of motion exercises, and progression of weight bearing status.  Surgical Treatment Operative treatment of Achilles tendon ruptures involves opening the skin and identifying the torn tendon. This is then sutured together to create a stable construct. This can be performed through a standard Achilles tendon repair technique or through a mini-incision technique (to read about the different types of techniques, look under ?Procedure? in Achilles Tendon Repair). By suturing the torn tendon ends together, they maintain continuity and can be mobilized more quickly. However, it is critical to understand that the return to normal activities must wait until adequate healing of the tendon has occurred. The potential advantages of an open repair of the Achilles tendon include, faster recovery, this means that patients will lose less strength. Early Range of Motion. They are able to move the ankle earlier so it is easier to regain motion. Lower Re-rupture Rate. The re-rupture rate may be significantly lower in operatively treated patients (2-5%) compared to patients treated non-operatively (8-15%). The main disadvantage of an open repair of the Achilles tendon rupture is the potential for a wound-healing problem which could lead to a deep infection that is difficult to eradicate, or a painful scar. Prevention To prevent Achilles tendonitis or rupture, the following tips are recommended. Avoid activities that place an enormous stress on the heel (for example, uphill running or excessive jumping). Stop all activity if there is pain at the back of the heel. If pain resumes with one particular exercise, another exercise should be selected. Wear proper shoes. Gradually strengthen calf muscles with sit-ups if prior episodes of Achilles tendonitis have occurred. Always warm up with stretching exercises before any activity. Avoid high-impact sports if prior episodes of Achilles tendon injury.
Surgical Treatment Operative treatment of Achilles tendon ruptures involves opening the skin and identifying the torn tendon. This is then sutured together to create a stable construct. This can be performed through a standard Achilles tendon repair technique or through a mini-incision technique (to read about the different types of techniques, look under ?Procedure? in Achilles Tendon Repair). By suturing the torn tendon ends together, they maintain continuity and can be mobilized more quickly. However, it is critical to understand that the return to normal activities must wait until adequate healing of the tendon has occurred. The potential advantages of an open repair of the Achilles tendon include, faster recovery, this means that patients will lose less strength. Early Range of Motion. They are able to move the ankle earlier so it is easier to regain motion. Lower Re-rupture Rate. The re-rupture rate may be significantly lower in operatively treated patients (2-5%) compared to patients treated non-operatively (8-15%). The main disadvantage of an open repair of the Achilles tendon rupture is the potential for a wound-healing problem which could lead to a deep infection that is difficult to eradicate, or a painful scar. Prevention To prevent Achilles tendonitis or rupture, the following tips are recommended. Avoid activities that place an enormous stress on the heel (for example, uphill running or excessive jumping). Stop all activity if there is pain at the back of the heel. If pain resumes with one particular exercise, another exercise should be selected. Wear proper shoes. Gradually strengthen calf muscles with sit-ups if prior episodes of Achilles tendonitis have occurred. Always warm up with stretching exercises before any activity. Avoid high-impact sports if prior episodes of Achilles tendon injury.
Non Insertional Achilles Tendonitis
 Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Achilles tendonitis is inflammation of the tendon, usually resulting from overuse associated with a change in playing surface, footwear or intensity of an activity. The Achilles tendon is surrounded by a connective tissue sheath (paratenon, or 'paratendon'), rather than a true synovial sheath. The paratenon stretches with movement, allowing maximum gliding action. Near the insertion of the tendon are two bursae - the subcutaneous calcaneal and the retrocalcaneal bursae.
Causes
Unusual use or overuse of the lower leg muscles and Achilles tendon is usually the cause of Achilles tendinitis. Repetitive jumping, kicking, and sprinting can lead to Achilles tendinitis in both recreational and competitive athletes. Runners, dancers, and athletes over age 65 are especially at risk. Sudden increases in training or competition can also inflame your Achilles tendon. For example, adding hills, stair-climbing, or sprinting to your running workout puts extra stress on your Achilles tendon. Improper technique during training can also strain the tendon. Intense running or jumping without stretching and strengthening your lower leg muscles can put you at risk regardless of your age or fitness level. Running on tight, exhausted, or fatigued calf muscles can put added stress on your Achilles tendon, as your tendon may not be ready to quickly start a workout after a period of inactivity. Direct blows or other injuries to the ankle, foot, or lower leg may pull your Achilles tendon too far and stretch the tissue. A hard contraction of the calf muscles, such as can happen when you push for the final sprint in a race, can strain the tendon. People whose feet roll inward, a condition called overpronation, are particularly at risk. Sometimes, shoes with too much heel cushioning put extra strain on the Achilles tendon.
Symptoms
Signs and symptoms of Achilles Tendinitis generally include pain and stiffness along your achilles tendon, especially in the morning. Pain in the back of your heel that gets worse with activity. Severe pain the day after exercising. Swelling that gets worse with activity. If you feel a pop in the back of your heel or bottom of you calf, you may have ruptured or torn you achilles tendon.
Diagnosis
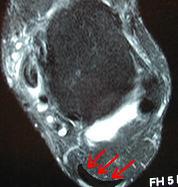
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
Achilles tendonitis will often respond to rest or changes in activity, stretching, or ice after activity. Non-steroidal anti- inflammatory drugs (NSAIDs), such as ibuprofen or naproxen may also help. Physical therapy focusing on stretching and strengthening, massage, alternating hot and cold baths, and ultrasound or sound waves can also help with healing and comfort. The temporary use of a heel lift or the insertion of an arch support, called an orthotic, into the shoe or sneaker can also help. Although seldom necessary, the ankle may be kept in a short leg cast or splint. Surgery is rarely needed but can remove bone spurs or the bony prominence of the heel bone. The injection of corticosteroids such as cortisone into the area of the Achilles tendon is usually avoided because it may cause the tendon to rupture.
Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
The following measures can significantly reduce the risk of developing Achilles tendonitis. Adequately stretch and warm up prior to exercise. Warm down and stretch after exercise. Choose footwear carefully and use footwear appropriate to the sport being undertaken. Use orthotic devices in footwear to correctly support the foot. Exercise within fitness levels and follow a sensible exercise programme. Develop strong, flexible calf muscles.
What Can You Do About Fallen Arches?

A variety of foot problems can lead to adult acquired flatfoot deformity (AAFD), a condition that results in a fallen arch with the foot pointed outward. Most people - no matter what the cause of their flatfoot - can be helped with orthotics and braces. In patients who have tried orthotics and braces without any relief, surgery can be a very effective way to help with the pain and deformity. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided.
Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side.
Symptoms
Flat feet don't usually cause problems, but they can put a strain on your muscles and ligaments (ligaments link two bones together at a joint). This may cause pain in your legs when you walk. If you have flat feet, you may experience pain in any of the following areas, the inside of your ankle, the arch of your foot, the outer side of your foot, the calf, the knee, hip or back. Some people with flat feet find that their weight is distributed unevenly, particularly if their foot rolls inwards too much (overpronates). If your foot overpronates, your shoes are likely to wear out quickly. Overpronation can also damage your ankle joint and Achilles tendon (the large tendon at the back of your ankle).
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
Non Surgical Treatment
Physiotherapists will carry out a detailed biomechanical assessment of your feet and lower limb. Once the causes have been identified a number of treatment methods may be used to help relieve pain and restore function in the feet including the use of custom made orthotics to support the foot and offload the areas which are painful, strengthening exercises for weakened muscles and tendons in the arch, and massage and mobilisation techniques to help mobilise stiff tissue and joints in the foot.
Surgical Treatment

Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths, also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Pain In The Arches Reasons Indicators And Treatment Options
Flat feet, also known as ?fallen arches? are often viewed as problematic simply because they look abnormal, the main arch of the foot, the medial longitudinal arch, has collapsed. Though flat feet are by no means normal, they are often the result of some other underlying condition or weakness rather than a problem with the actual arch itself that has collapsed. Conventional treatment involving foot support either via supportive footwear, orthotics, or some other bracing system is usually more disadvantageous than beneficial and surgery is rarely the answer.

Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape.
Symptoms
Pain in arch of foot is really the only symptom of this condition. It is unlikely to see any swelling or bruising and instead there will be a deep tender spot near the heel. Occasionally the pain may radiate further down the foot. With this condition, pain will usually be felt first thing in the morning or after periods of sitting. This is because the plantar fascia tightens and shortens slightly when there is no weight on it and by standing on it it suddenly stretches and becomes painful. After a few steps it starts to loosen off and the pain may subside. If this is the same pattern of pain you experience it is quite likely you have plantar fasciits. Pain may also be felt when walking up stairs or standing on tip-toes (anything that stretches the fascia).
Diagnosis
The doctor will take a brief history to determine how the injury occurred. If necessary, a thorough physical exam may be conducted to evaluate for any other injuries. Taking your workout shoes to the exam may also provide valuable information to the medical practitioner. Both feet will be physically and visually examined by the medical practitioner. The foot and arch will be touched and manipulated possibly with a lot of pressure and inspected to identify obvious deformities, tender spots, or any differences in the bones of the foot and arch.
Non Surgical Treatment
There is considerable debate about the best treatment option for plantar fasciitis. Some authors suggest all of the 'mainstream' methods of treatment don't actually help at all and can actually make the symptoms worse. However, on the whole, there are several of the most commonly cited treatment options for plantar fasciitis and these are generally accepted throughout the medical community. I would recommend giving these options a try if you haven't already. Rest. This is mainly applicable to the sports people as rest is possible treatment. (For those who cannot rest e.g. people who work on their feet - skip to the other treatment options below). Rest until it is not painful. This is made more difficult as people need to use their feet to perform daily activities but certainly stop sporting activities that are likely to be putting the fascia under excessive stress. Perform Self Micro-Massage (you can watch this video by clicking the link or scrolling further down the page as it's embedded on this lens!) This massage technique is used to break down fibrous tissue and also to stimulate blood flow to the area, both of which encourage healing and reduce pain. There is also a potentially soothing effect on nerve endings which will contribute to pain relief. Ice/Cold Therapy. Particularly useful after spending periods on your feet to reduce the inflammation. Wrap some ice or a bag of frozen peas in a towel and hold against the foot for up to 10 minutes. Repeat until symptoms have resolved. Heat Therapy. Heat therapy can be used (not after activity) to improve blood flow to the area to encourage healing. A heat pack of hot water bottle can be used. 10 minutes is ideal. Careful not to burn yourself. A good taping technique. By taping the foot in a certain way you can limit the movement in the foot and prevent the fascia from over-stretching and gives it a chance to rest and heal. Click on the link for more information on taping techniques. Weight Management. If you are over-weight, any weight you can loose will help to ease the burden on your sore feet and plantar fascia. Orthotic devices (often mis-spelled orthodic) are special insoles that can be used to limit over-pronation (discussed earlier) and control foot function. By preventing the arches flattening excessively, the plantar fascia is not over-stretched to the same extent and this should help with the symptoms and encourage healing. Stretching the calf muscles (again, click this link or scroll to the bottom of the page to watch the embedded video) can help to lengthen these muscles and the Achilles tendon - a risk factor for plantar fasciitis. Stretching of the plantar fascia itself is also encouraged, particularly before getting up the morning (night splints can be used for this effect) and after periods of rest. This can be achieved by placing a towel or band under the ball of the foot and gently pulling upwards until a stretch is felt. Hold for about 15-20 seconds then rest briefly. Repeat 2-3 times. As you can see there are many different treatment options available. Try incorporating some of these in to your daily routine and see what works for you. Regardless of the method the main aim is to prevent the fascia from over-stretching. Medical professionals such as a Podiatrist may decide to make custom orthotics or try ultra-sound therapy. It is likely that anti-inflammatory medications will also be recommended. If you have tried the treatment options and your symptoms persist I'd recommend going to see a medical professional for further advice.

Surgical Treatment
The soft tissue surgeries usually would include a lengthening of the Achilles tendon, releasing of the plantar fascia as well as tendon transfers. These procedures are usually done in conjunction with bony procedures such as calcaneal osteotomies (to lower the heel bone and get it more under the leg itself), as well as metatarsal osteotomies. These procedures usually involve either cutting or fusion of the bones, and placement of fixation devices to allow the bones to heal. Healing time is usually at least 6-8 weeks and usually the patient must be non-weight bearing during the healing process. These types of surgical corrections are usually reserved for the more difficult, painful and deformed feet. They can require more surgeries down the line. These procedures are usually the last resort after all other modes of treatment have been exhausted (except in children where it is usually best to treat the deformity early). There are many different degrees of high arched feet and these procedures should be left for the more extreme cases. These cases usually require a very high degree of surgical skill and should only be done by those who frequently perform these types of cases.
Prevention
The best method for preventing plantar fasciitis is stretching. The plantar fascia can be stretched by grabbing the toes, pulling the foot upward and holding for 15 seconds. To stretch the calf muscles, place hands on a wall and drop affected leg back into a lunge step while keeping the heel of the back leg down. Keep the back knee straight for one stretch and then bend the knee slightly to stretch a deeper muscle in the calf. Hold stretch for 15 seconds and repeat three times.
Stretching Exercises
Strengthening exercises. Below are two simple strength exercises to help condition the muscles, tendons and joints around the foot and ankle. Plantar Rolling. Place a small tin can or tennis ball under the arch of the affected foot. Slowly move the foot back and forth allowing the tin can or tennis ball to roll around under the arch. This activity will help to stretch, strengthen and massage the affected area. Toe Walking. Stand upright in bare feet and rise up onto the toes and front of the foot. Balance in this position and walk forward in slow, small steps. Maintain an upright, balanced posture, staying as high as possible with each step. Complete three sets of the exercise, with a short break in between sets, for a total of 20 meters.
What precisely is Adult Aquired Flat Foot ?
Adult-acquired flatfoot or even collapsed arch occurs because the huge tendon around the inside of the ankle - the posterior tibial tendon - gets stretched out as well as no longer sports ths foot?s arch. in many cases, the situation worsens and and the tendon thickens, turning out in order to be painful, particularly during activities. Flatfoot or perhaps collapsed arch is also referred to as posterior tibial tendon dysfunction. This kind of issue is unique when compared with getting flat feet since birth (known as congenital flatfoot), although sometimes these patients develop similar signs and symptoms along with require comparable treatments.

Causes
The most common trigger involving acquired adult flatfoot is actually posterior tibial tendon dysfunction. What leads to adult acquired flat foot? Fracture or perhaps dislocation. Tendon laceration. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
The 1st stage represents inflammation and also symptoms originating through an irritated posterior tibial tendon, that is still functional. Stage a pair of is actually characterized by a change within the alignment in the foot noted in observation although standing (see higher than photos). Your deformity is actually supple meaning the foot will be freely movable plus a ?normal? position may be restored through the examiner. Stage a pair of can be related using the inability to perform a single-leg heel rise. Your third stage can be dysfunction in the posterior tibial tendon is a flatfoot deformity that gets in order to be stiff simply because of arthritis. Prolonged deformity leads to irritation to the involved joints causing arthritis. The Actual fourth cycle is a flatfoot deformity possibly supple (stage two) as well as stiff (stage 3) using involvement with the ankle joint. This kind of occurs once the deltoid ligament, the particular major supporting composition about the inside of the ankle, doesn't offer support. the ankle gets in order to be unstable and will demonstrate any tilted appearance about X-ray. Failure with the deltoid ligament comes from an inward displacement regarding the load bearing forces. While prolonged, this alter can easily result in ankle arthritis. The Actual great majority associated with patients with acquired adult flatfoot deformity are stage 2 once that they seek remedy from a physician.
Diagnosis
First, each feet should be looked at using the affected person standing and the entire lower extremity visible. The Particular foot needs in order to be inspected via over too as coming from behind the patient, as valgus angulation in the hindfoot is better appreciated if the foot is actually viewed via behind. Johnson described the particular so-called more-toes sign: with additional advanced deformity along with abduction of the forefoot, more of the lateral toes grow to be noticeable when the foot is actually viewed via behind. The Particular single-limb heel-rise test is an superb determinant with the operate in the posterior tibial tendon. Your patient will be asked to try to rise onto the ball of one foot while the other foot can be suspended off the floor. under normal circumstances, the posterior tibial muscle, which inverts as well as stabilizes your hindfoot, can be activated as the affected person actually begins to rise onto the forefoot. the gastrocnemius-soleus muscle mass team then elevates the actual calcaneus, and furthermore the heel-rise is accomplished. with dysfunction of the posterior tibial tendon, however, inversion of the heel can be weak, and also either the heel remains throughout valgus or the individual is actually not in the position to rise to the forefoot. In your event that the patient may execute a single-limb heel-rise, the limb might always be stressed further by asking the patient to execute this maneuver repetitively.
Non surgical Treatment
Because in the progressive nature of PTTD, early therapy can be advised. In the actual event that treated early enough, your signs could resolve without the actual requirement for surgery along with progression of one's situation may be arrested. Inside contrast, untreated PTTD could depart anyone with an very flat foot, painful arthritis within the foot along with ankle, as well as increasing limitations upon walking, running, or another activities. Inside many cases associated with PTTD, treatment can easily start out with non-surgical approaches in which might include. Orthotic devices as well as bracing. In Order To give the arch the particular assistance it needs, your foot and also ankle surgeon might offer a person with an ankle brace or perhaps a custom orthotic device that fits into the shoe. Immobilization. Sometimes the short-leg cast or even boot is actually worn to immobilize the particular foot and permit the particular tendon for you to heal, or even you might must entirely steer clear of almost all weight-bearing for a while. Physical therapy. Ultrasound therapy and also exercises may aid rehabilitate the actual tendon along with muscle mass following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, aid reduce the pain sensation as well as inflammation. Shoe modifications. Your Own foot along with ankle surgeon might advise changes to make together with your shoes and could supply particular inserts designed to improve arch support.

Surgical Treatment
Until recently, operative remedy has been indicated for most patients with stage two deformities. However, with the use associated with potentially effective nonoperative management , operative treatment method is currently indicated for anyone patients that have failed nonoperative management. The Particular rules involving operative therapy of stage 2 deformities contain transferring an additional tendon to help serve your role of the dysfunctional posterior tibial tendon (usually the particular flexor hallucis longus can be transferred). Restoring the actual shape along with alignment in the foot. This moves the body weight bearing axis back to the center of the ankle. Changing the actual model of the actual foot may be practiced through one as well as more of your following procedures. cutting the actual heel bone along with shifting it towards the inside (Medializing calcaneal osteotomy). Lateral column lengthening restores the actual arch along with general alignment of the foot. Medial column stabilization. This specific stiffens the ray involving the big toe to better support the arch. Lengthening of the Achilles tendon or perhaps Gastrocnemius. This will permit the ankle to go adequately as quickly as your alignment with the foot is actually corrected. Stage 3 acquired adult flatfoot deformity is treated operatively with a hindfoot fusion (arthrodesis). This is completed with either the double or even triple arthrodesis - fusion of a pair of as well as three with the joints in hindfoot via which in turn the actual deformity occurs. It is very important each occasion a hindfoot arthrodesis is performed that will it's done inside such a method throughout which the particular underlying foot deformity is corrected first. simply fusing your hindfoot joints in position can be will zero longer acceptable.
Arch Pain Cause And Effect
Flat feet and fallen arches are terms used to describe lowering of the long inner arch of the foot. In the past, we thought that flat feet were a sign of a poorly developed or poorly structured foot. Now we know that people with flat feet function generally well and that flat feet don?t cause many foot problems. The most important factor in foot soreness and injury is not how flat or high your arches are, but the way you walk and move. If your feet move abnormally while you are walking or standing, this can make you more prone to injuries and foot soreness.

Causes
There are a number of possible causes for arch pain, but the most common are structural imbalances of the foot, such a pronated foot (rolls inward at the ankles). This is often not enough in isolation to cause the problem, but in combination with other factors arch pain may develop. These other factors are usually associated with overuse - running, walking, hard surfaces and/or OFAD (on feet all day), usually combined with inadequate or non-supportive footwear. The more common specific causes of arch pain can be plantar fasciitis (strain of the plantar fascia - a strong ligament that supports the arch), tarsal tunnel syndrome (a pinched nerve at the ankle that refers pain to the arch), foot strain from a pronated foot or flat foot, there can be osteoarthritis of the joints in the midfoot that can cause arch pain.
Symptoms
People suffering from pain in the arch sometimes complain of burning or soreness on the foot sole, which is worse in the morning and after physical activity. There may also be some tenderness when pressure is applied to the sole of the foot or heel. In addition to this, patients tend to complain of more pain when they stand on tiptoe.
Diagnosis
To come to a correct diagnosis, your podiatrist will examine your foot by using his or her fingers to look for a lump or stone bruise in the ball of your foot. He or she will examine your foot to look for deformities such as high or low arches, or to see if you have hammertoes. He or she may use x-rays, MRIs (magnetic resource imaging), and CT scans to rule out fractures and damage to ligaments, tendons, and other surrounding tissues. Your doctor will also inquire about your daily activities, symptoms, medical history, and family history. If you spend a lot of time running or jumping, you may be at a higher risk for pain in the bottom of your foot. These diagnostic tests will help your doctor come to a proper diagnosis and create an appropriate treatment plan.
Non Surgical Treatment
Doctors commonly prescribe shoe inserts, or orthotics, to support the arch. These devices make walking and standing more comfortable for a person with fallen arches, reports the American Academy of Orthopaedic Surgeons. Orthotics are typically worn with closed shoes. They are available over-the-counter or can be custom-made.

Surgical Treatment
Surgery may be necessary in situations where the symptoms are likely to get worse over time, or when pain and instability cannot be corrected with external orthopedic devices. There are many types of surgical procedures, including cavus foot reconstruction, which can be performed to correct the foot and the ankle and restore function and muscle balance.
Stretching Exercises
You may start exercising the muscles of your foot right away by gently stretching and strengthening them. Frozen can roll. Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if it is done first thing in the morning. Towel stretch. Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your leg straight. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Standing calf stretch. Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day. Seated plantar fascia stretch. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times. Plantar fascia massage. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.